Diabetes and its complications: a metabolomic intervention
Metabolic insight Feb 20, 2025

According to the International Diabetes Federation (IDF), half a million diabetes-related deaths were preventable in Europe in 2021. The IDF’s Regional Chair, Professor Nebojsa Lalic, compared this number to “three jumbo jets falling from the skies every single day”. Many of these deaths are preventable through changes in diet or exercise patterns, which is why it’s helpful to identify people at risk as early as possible.
Flagging the initial development of disease
An effective way to detect the risk of diabetes early is through Nightingale Health’s metabolomic blood profiling. Recently, we showed that we can identify a small group of individuals at six- to ten-fold risk of type 2 diabetes using metabolomic biomarkers from a single blood sample. By predicting the development of disease years before it happens, people are given time to implement lifestyle changes or receive preventative treatment.
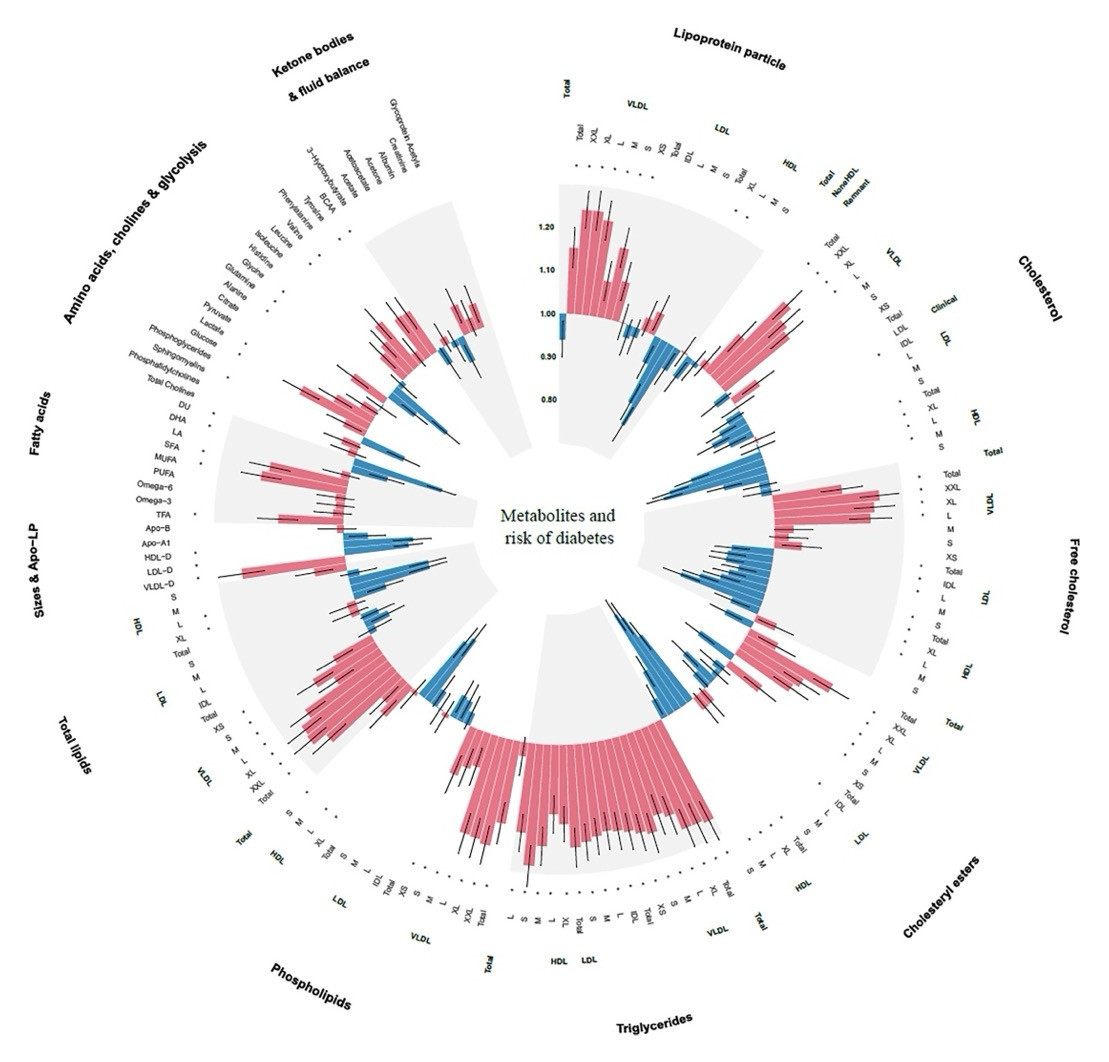
Figure 1. Associations of 168 metabolic biomarkers with risk of diabetes among 13,489 participants with prediabetes. Hazard ratios (HRs) were presented per 1 standard deviation (SD) higher of metabolic biomarkers on the natural log scale and were adjusted for age, sex, ethnicity, education, Townsend Deprivation Index, employment status, household income, family history of diabetes, history of CVD, history of hypertension, history of dyslipidemia, history of CLD, history of cancer, body mass index, waist circumference, hip circumference, smoking status, moderate alcohol, healthy diet score, healthy sleep score, physical activity, systolic blood pressure, diastolic blood pressure, and glycated hemoglobin A1c. Source: Li et al., 2024.
Preparing for progression
Individuals who already have a higher-than-normal blood sugar level but do not yet have type 2 diabetes, can be diagnosed with “prediabetes”. A recent study found that the metabolomic profiles of those individuals can be used to predict whether they are more or less likely to progress to a type 2 diabetes diagnosis in the future (Figure 1). The figure depicts the range of different biomarkers associated with disease progression. In other words, even when someone is already at high risk, their metabolome still contains information about their future disease trajectory.
Metabolomic profiles not only provide an early warning of the initial onset of disease and the progression of prediabetes, but also signal the development of future complications among those who already have type 2 diabetes. Utilizing UK Biobank data from people previously diagnosed with diabetes, we developed models that estimate the risk of further complications, including eye disorders, kidney disease, cardiovascular events, and death, up to ten years after the initial diagnosis. In our analyses, more than a third of individuals with type 2 diabetes experienced complications within ten years. By investigating their metabolomic profiles, we found progression signatures that increased an individual’s risk of complications – two-fold for cardiovascular events and almost five-fold for kidney disease.
Healthcare professionals currently have a few commonly used clinical chemistry measures at their disposal to assess diabetes severity and expected progression, such as cholesterol, triglycerides, creatinine, and hemoglobin A1c (HbA1c). When comparing Nightingale Health’s metabolomic biomarkers to these commonly used clinical measures, the metabolomic biomarkers perform similarly or better in all cases.
A metabolomic intervention
In summary, metabolomic models can help predict not just who might develop type 2 diabetes, but also the likelihood of experiencing complications. Metabolomic profiles can identify early warning signs and outperform models based on traditional clinical measures. Incorporating metabolomics into clinical care could enable earlier interventions and more personalized treatment strategies. By identifying specific risks, healthcare providers can focus resources where they are most needed, with the aim of improving outcomes for all patients.
References
Nightingale Health Biobank Collaborative Group. Metabolomic and genomic prediction of common diseases in 700,217 participants in three national biobanks. Nat. Commun. 15, 10092 (2024).
IDF Europe. Type 2 Diabetes: A Preventable Catastrophe? A Call to Action by IDF Europe.https://idf.org/europe/media/uploads/sites/2/2023/06/IDF-Europe_Type-2-Diabetes.-A-preventable-catastrophe.pdf (2023).
Li, J. et al. Nuclear magnetic resonance-based metabolomics with machine learning for predicting progression from prediabetes to diabetes. eLife 13, RP98709 (2024).
