Metabolic insights: Nightingale's biomarkers in smoking and lung cancer risk
Data Sep 27, 2023
“The results highlight that Nightingale’s biomarkers provide a quantitative proxy for smoking exposure and may be used as a tool for predicting smoking-related disease risk.”
Smoking is well known as a dramatic risk factor for chronic diseases like lung cancer, chronic obstructive pulmonary disease (COPD), and heart disease. It also increases the risk of many other diseases to different degrees and is in general one of the most important covariates in epidemiological analyses.
Smoking behavior is most often assessed using questionnaire-based categorical variables (e.g., current smoker / never smoked) or self-estimated quantitative measures (e.g., the number of cigarettes smoked per day). However, the reliability and availability of these variables is limited in many cohorts. It is possible to directly measure biomarkers of nicotine metabolism, such as cotinine, but collecting a sample and taking this measurement is typically only done in studies specifically focused on smoking itself.
Another possibility is to use general-purpose blood metabolites to estimate smoking behavior. Here we explore associations of Nightingale’s blood biomarkers with smoking and consider how they can be used to capture this exposure.
Smoking is associated with fatty acids and chronic inflammation
To assess the associations of biomarkers with smoking, we utilized metabolomic data obtained from Nightingale Health's platform, comprising data from over 270,000 UK Biobank samples. We computed associations of 251 blood biomarkers with smoking status and adjusted for age, sex, body-mass index, and cholesterol medication.
Our analysis revealed widespread associations between smoking status and biomarkers, consistent with the expectation that it perturbs many aspects of normal metabolism. Fatty acids exhibited the strongest associations, for example an odds ratio (OR) of 0.58 (0.58-0.59 95% CI) for the ratio of polyunsaturated and monounsaturated fatty acids and 0.64 (0.64-0.65 95% CI) for percentage Omega-3 fatty acids. These findings are particularly intriguing given the growing scientific evidence implicating that fatty acids play a causal role in various diseases (Davyson et al. 2023, He et al. 2022, Li et al. 2022). Additionally, we observed substantial, unfavorable associations with a biomarker of chronic inflammation, Glycoprotein acetyls (GlycA), which exhibited an OR of 1.50 (95% CI: 1.48-1.52). Figure 1 shows how long-term smokers show a distorted metabolic profile across nearly all the key functions captured by our biomarkers.
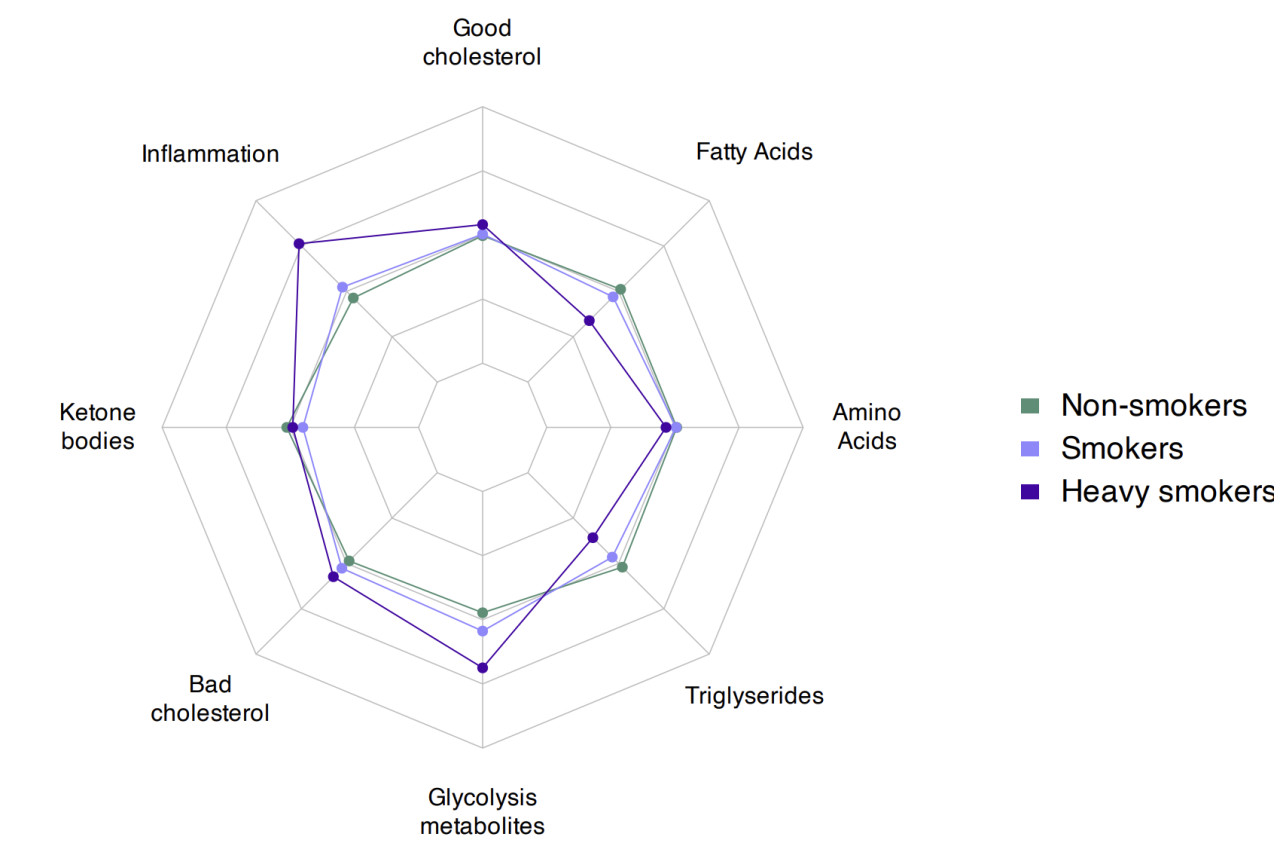
Figure 1. Average metabolomic profiles of non-smokers, smokers, and heavy smokers with over 60 pack-years of smoking show distinct patterns captured by the main components of metabolome (via sparse factor analysis).
Predicting lung cancer risk
To assess the value of using Nightingale’s biomarkers as a proxy for true smoking exposure in a disease study, we compared a multi-biomarker score to pack-years of smoking in predicting the risk of lung cancer over the next two years. The figure below shows how Nightingale’s biomarkers exhibit about twice the predictive performance when compared to pack-years of smoking. However, the best predictive performance was achieved when combining these two sources of information. More information on disease prediction with metabolomic biomarkers can be found from our latest pre-print Metabolomic and genomic prediction of common diseases in 477,706 participants in three national biobanks.
These results highlight that Nightingale’s biomarkers provide a quantitative proxy for smoking exposure and may be used as a tool for predicting smoking related disease risk.
If interested in exploring blood biomarkers in your cohort, please email us at research@nightingalehealth.com.

Figure 2. Associations of pack-years of smoking, Nightingale’s multi-biomarker score and their combination with lung cancer over 2 years of follow-up. Associations were computed within previous and current smokers adjusting for age, sex and smoking status. HR = hazard ratio, CI = confidence interval.
