The hidden spectrum of risk in people with moderately increased blood pressure
Data Dec 07, 2023

Nearly a third of adults in the UK have high blood pressure, which is a risk factor for cardiovascular diseases like heart attack and stroke. In this research blog post, our scientists learned from the UK Biobank data how blood biomarkers can help identify the individuals with moderately increased blood pressure who would benefit most from treatment.
High blood pressure is a risk factor for adverse cardiovascular outcomes like heart attack and stroke. Nearly a third of adults in the UK have high blood pressure, but fortunately, proper treatment with widely available medicines can lower blood pressure and prevent adverse cardiovascular outcomes.
According to the guidelines developed for the UK, persistent high blood pressure is defined as having a systolic pressure greater than 140 mmHg or a diastolic pressure greater than 90 mmHg when measured at a health clinic. Those with the highest category of blood pressure (>180/120 mmHg) are recommended for immediate specialist consultation, while those with blood pressure of 160-180/100-120 mmHg should always be offered antihypertensive medication, and those with blood pressure of 140-159/90-99 mmHg be offered such medicine only in the presence of a comorbidity such as diabetes or kidney disease. Individuals with only slightly elevated blood pressure (130-139/85-89 mmHg) are encouraged to make lifestyle changes including reducing their intake of salt and alcohol to lower their blood pressure.
Blood pressure is a dose-dependent risk factor for cardiovascular disease
This “ladder” of increasingly urgent recommendations is based on the dose-dependent relationship between blood pressure and cardiovascular disease risk. In other words, there’s not just one line between “high” and “low” — the higher you go, the more your risk increases. Figure 1 shows this relationship in 500,000 UK Biobank participants by comparing the 10-year incidence of major cardiovascular events (cardiovascular death, nonfatal myocardial infarction, and nonfatal stroke) in different blood pressure categories¹. Compared to those with so-called “optimal” blood pressure (< 120/80 mmHg), those with slightly elevated blood pressure of 130-139/85-89 had an increased 10-year hazard ratio (HR) of 1.3, while those in the highest category (>180/120) had an HR of 2.6. This result is concordant with previously published findings that individuals with only slightly elevated blood pressure are at meaningfully increased risk, and yet are typically not treated. Understanding whether it’s possible to stratify this group further, to identify and treat those at greatest risk, is especially important because it is so common: this group represents a third of the adults in the UK Biobank.
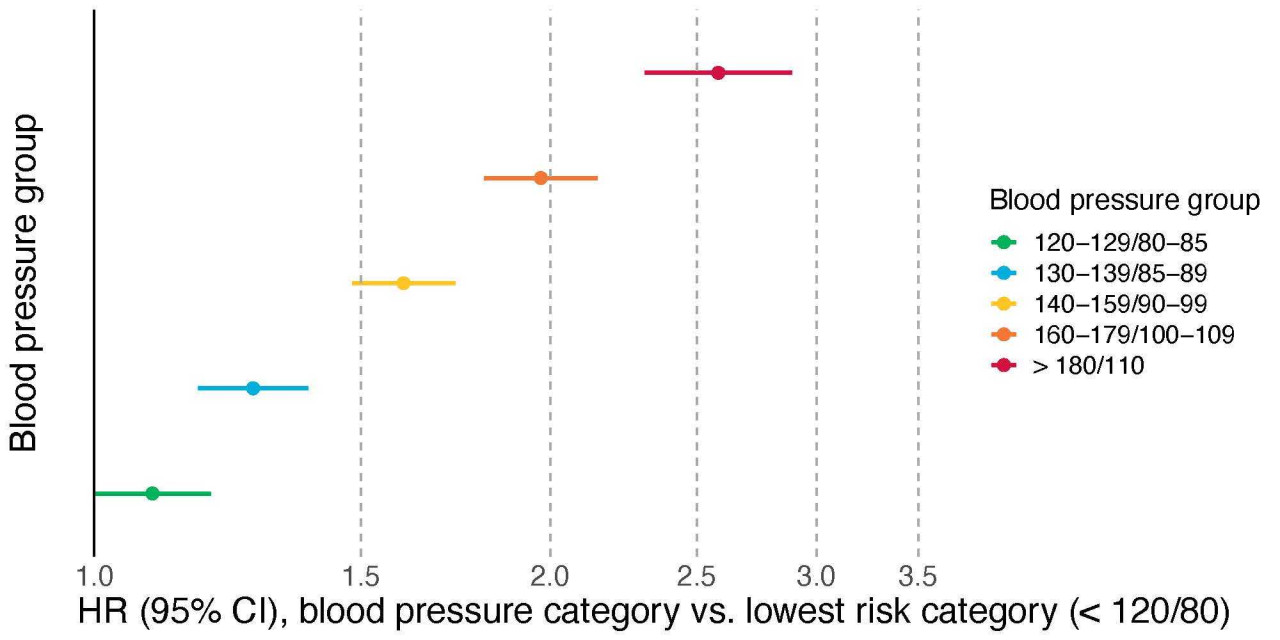
Figure 1. Blood pressure category is associated with major cardiovascular events in a dose-dependent manner.
Blood biomarkers predict cardiovascular disease in individuals with slightly elevated blood pressure
We examined whether Nightingale’s blood biomarkers could predict which individuals with slightly or moderately elevated blood pressure (130-159/85-99 mmHg, yellow and blue dots in Figure 1) were at highest risk of severe cardiovascular events. We built an overall cardiovascular disease risk score that combines information from many different biomarkers². When we divided these two blood pressure groups into those with the highest 10% of our biomarker score and the remaining 90%, we discovered these two groups have dramatically different risk (Figure 2). Individuals with slightly elevated blood pressure (130-139/85-89 mmHg) but not in the high metabolomic risk group (light blue dot in Figure 2) had no significant excess risk compared to individuals with optimal blood pressure, and even those with moderately increased blood pressure (140-159/90-99 mmHg, yellow dot in Figure 2) had only slightly elevated risk (HR = 1.4). By contrast, those in these intermediate blood pressure groups but in the top 10% of metabolomic risk (dark blue and brown dots in Figure 2) had even greater risk than the highest blood pressure group overall.
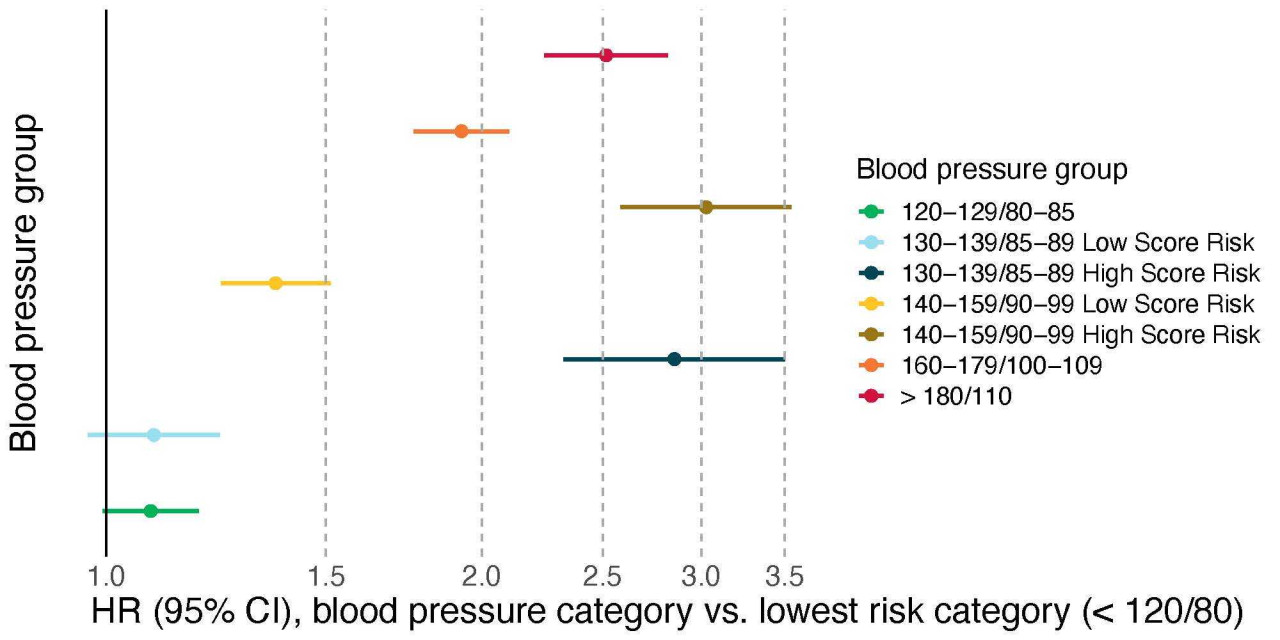
Figure 2. The Nightingale biomarker risk score dramatically stratifies the cardiovascular risk of individuals with intermediate or slightly elevated blood pressure.
